
.png)
Understanding the customer journey is essential to providing a seamless and positive user experience. We identified five critical phases that customers typically go through: Onboarding, Research on Options, Service Engagement, Troubleshoot, and Claims Submission.

As employees start their new job or students start at a university and receive their orientation package, they feel overwhelmed and confused about the various coverage options available to them. Addressing this confusion early and providing clear information about coverage options,can help them make informed decisions and feel supported in their journey.
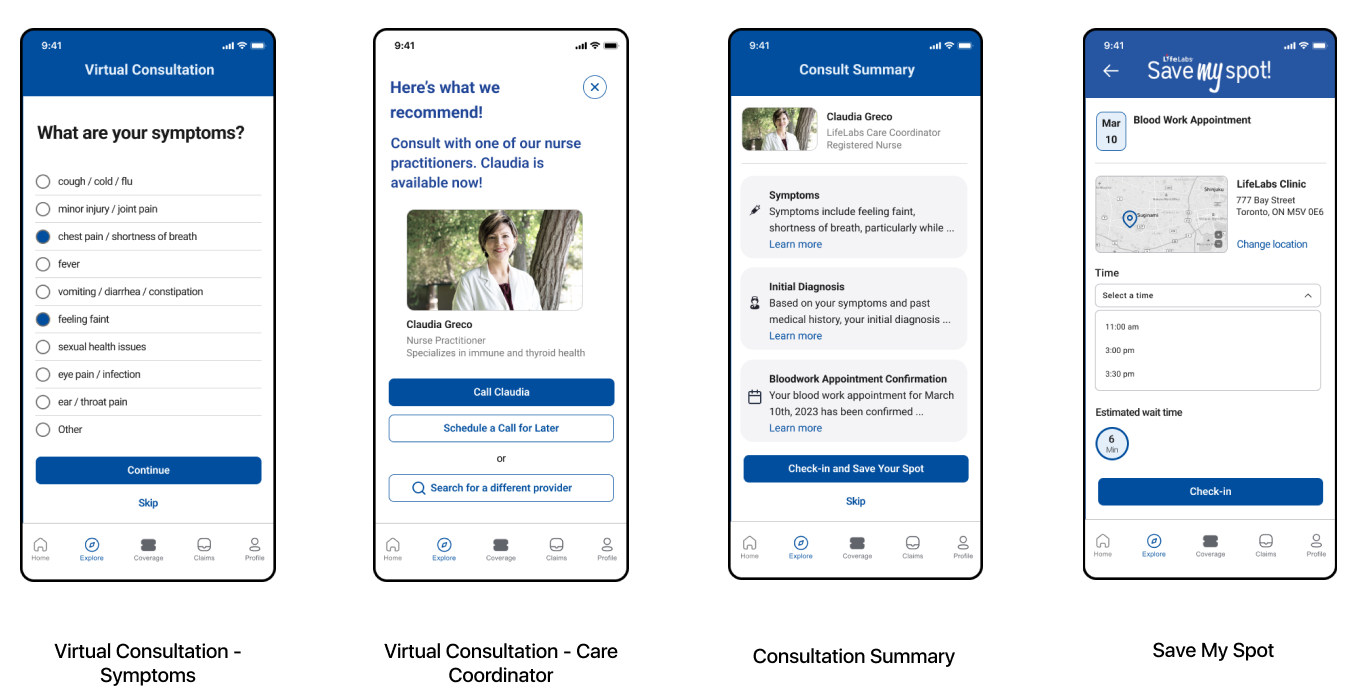
Users face difficulties when seeking referrals and urgent care which often requires them to visit multiple healthcare facilities. They also expressed frustration with appointment wait times and the lack of digital support. The goal is to offer digital solutions that streamline the process and reduce the need for physical visits, thereby increasing convenience for users seeking urgent care and referrals.
Finding #1
To better understand how users want to select a plan and what about their plan would they want to learn about as well as how, we used lo-fi screens and prompts to facilitate the co-design session. We learnt that users wanted a fast, simple onboarding with a quiz-style questionnaire, more customization, a benefits summary and better findability.
Finding #2
We found that users look for a variety of criteria when choosing a service provider, prefer reduced steps when booking an appointment and favor digital support over in-person assistance wherever possible.
By leveraging LifeLab's ecosystem of existing products and features, we are confident that we can increase activation and utilization rates, boost customer satisfaction, and help customers take control of their health and well-being.
Service Outcome: User has greater control over their coverage options and feels they are getting better value from their plan
Business Outcome: Automating onboarding to reduce manual and inconsistent processesIncreased enrolment and access to user data
Service Outcome: User has a clearer understanding of their insurance coverage and how to use it since they have better access to information - all in one place.
Business Outcome: Increased customer satisfaction and retention

Service Outcome: Users can skip the inconvenience of visiting multiple healthcare facilities to obtain a referral or appointment by taking advantage of virtual consultations. Additionally they can bypass wait times by utilizing the ‘Save my Spot’ feature.
Business Outcome: Leverage existing LifeLab infrastructure to offer convenient health care to customers (Save My Spot and virtual health consultations) helps
increase utilization rate and customer satisfaction + retention.
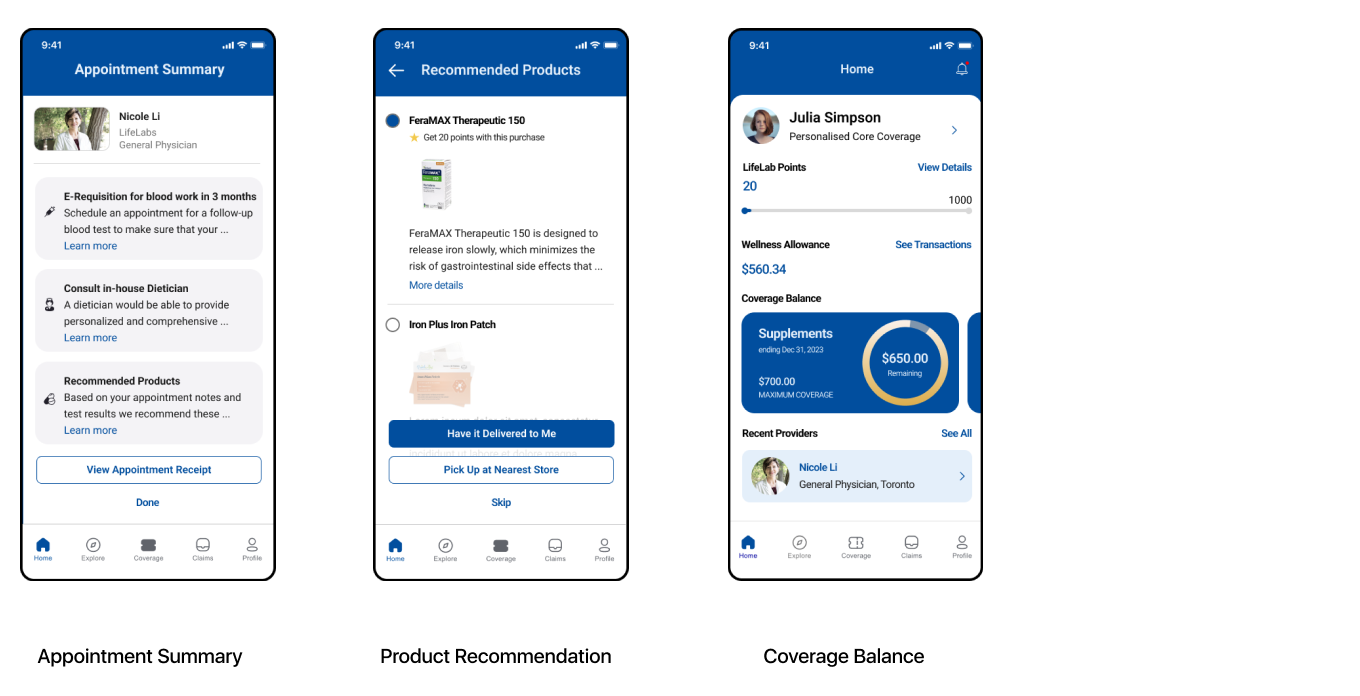
Service Outcome: Users get personalized recommendations on follow-up appointments and products to purchase based on their appointment results along with access to “one-stop-shop” service.
Business Outcome: Leverage existing LifeLab infrastructure to offer convenient health care to customers (Save My Spot and virtual health consultations) helps
increase utilization rate and customer satisfaction + retention.
By leveraging LifeLab's ecosystem of existing products and features, we are confident that we can increase activation and utilization rates, boost customer satisfaction, and help customers take control of their health and well-being.
